The human organism possesses an intricate and highly evolved network of physiological responses designed to maintain internal equilibrium and ensure survival. Central to this network is the autonomic nervous system, a division of the peripheral nervous system that operates largely outside conscious control. Within the autonomic nervous system, two principal branches exist: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). While the PNS is often characterized as the “rest and digest” system, the SNS orchestrates the body’s acute stress response, often referred to as the “fight or flight” mechanism. The concept of a “sympathetic nervous system lock” refers to a state where the SNS remains chronically activated, leading to a cascade of physiological and psychological ramifications.
To comprehend the implications of a sympathetic nervous system lock, it is essential to first understand the fundamental mechanics of the fight or flight response. This primal survival mechanism is deeply rooted in humanity’s evolutionary history, designed to prepare the body for immediate action in the face of perceived danger. You can watch a fascinating documentary about the concept of lost time and its impact on our lives.
Neural Pathways and Neurotransmitters
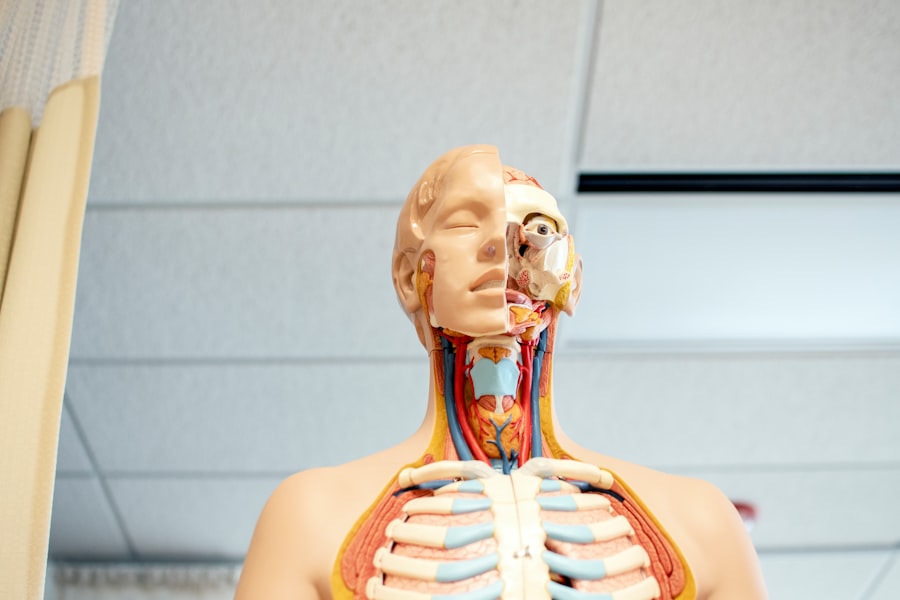
The initiation of the fight or flight response begins with the perception of a threat, which can be real or imagined. Sensory organs transmit this information to the brain, specifically to the amygdala, the brain’s alarm center. The amygdala, in turn, communicates with the hypothalamus, the command center for the autonomic nervous system.
- Hypothalamus: This small but mighty brain region activates the SNS by signaling to the adrenal glands, situated atop the kidneys.
- Adrenal Glands: These glands release a surge of powerful stress hormones into the bloodstream, primarily adrenaline (epinephrine) and noradrenaline (norepinephrine).
- Sympathetic Ganglia: The SNS utilizes a network of sympathetic ganglia, collections of nerve cell bodies, to rapidly transmit signals to various target organs and tissues throughout the body.
Physiological Manifestations
The release of adrenaline and noradrenaline triggers a rapid and profound re-prioritization of bodily functions, preparing the organism for intense physical exertion.
- Cardiovascular Changes: Heart rate and blood pressure increase dramatically, diverting blood flow to essential muscles and away from less critical functions like digestion. Imagine the body as a high-performance engine suddenly revving to its maximum capacity.
- Respiratory Adjustments: Bronchioles in the lungs dilate, increasing oxygen intake. Breathing becomes shallower and more rapid.
- Metabolic Shift: Glucose stores are released from the liver, providing an immediate energy boost to fuel muscle activity.
- Pupil Dilation: The pupils widen to enhance visual acuity, allowing for better perception of the environment.
- Gastrointestinal Shutdown: Digestive processes are suppressed, as energy is redirected towards immediate survival needs. This is why individuals under extreme stress often lose their appetite or experience stomach upset.
- Sweat Gland Activation: Increased perspiration helps to cool the body during intensified physical activity.
These synchronized physiological changes equip the individual to either confront the threat head-on (fight) or escape from it (flight).
The concept of sympathetic nervous system lock is intricately linked to various physiological responses in the body, particularly in relation to stress and anxiety. For a deeper understanding of how the sympathetic nervous system affects overall health and well-being, you can explore a related article that discusses these mechanisms in detail. To read more about this topic, visit this article.
The Path to Chronic Sympathetic Activation
While the acute fight or flight response is life-saving in genuine emergencies, prolonged or unremitting activation of the SNS constitutes a “sympathetic nervous system lock.” This occurs when the body remains in a state of high alert even in the absence of an immediate, tangible threat.
Stressors in Modern Life
Modern society, despite its advancements, presents a myriad of stressors that can persistently trigger the SNS. Unlike prehistoric threats, which were often discrete and ephemeral (e.g., encountering a predator), contemporary stressors are frequently chronic and less easily resolved.
- Work-Related Stress: Demanding jobs, long hours, perceived lack of control, and interpersonal conflicts in the workplace are common culprits.
- Financial Strain: Economic insecurity and debt can create a constant undercurrent of anxiety.
- Relationship Issues: Unresolved conflicts, strained family dynamics, or turbulent romantic relationships can be significant and ongoing sources of distress.
- Chronic Illness: Living with a chronic medical condition can impose a sustained burden on the body and mind, triggering compensatory SNS activation.
- Environmental Factors: Noise pollution, high-density living, and a constant influx of information can contribute to a hypervigilant state.
- Trauma: Past traumatic experiences, even if seemingly resolved, can embed a lasting imprint on the nervous system, making it more prone to SNS activation. This is analogous to an alarm system that remains overly sensitive after a break-in, constantly triggered by minor disturbances.
The Role of Perception and Interpretation
Crucially, the SNS response is not solely dictated by objective reality but also by individual perception and interpretation of events. What one person perceives as a minor inconvenience, another might experience as an overwhelming threat.
- Cognitive Appraisal: Our thoughts, beliefs, and expectations significantly influence how we appraise situations. Catastrophizing or pessimistic thinking can amplify the perceived threat, thereby intensifying the SNS response.
- Learned Helplessness: Prolonged exposure to uncontrollable stressors can lead to a state of learned helplessness, where individuals feel powerless to alter their circumstances, further entrenching SNS activation.
- Personality Traits: Certain personality traits, such as neuroticism or high-trait anxiety, can predispose individuals to a more reactive SNS.
Consequences of a Sympathetic Nervous System Lock
A sustained state of sympathetic activation exacts a heavy toll on the body and mind, leading to a wide array of adverse health outcomes. The body is not designed for perpetual emergency mode; it requires periods of rest and repair facilitated by the PNS.
Physical Health Impacts
The chronic hyperarousal associated with a sympathetic nervous system lock can manifest in numerous physical ailments. It is akin to continuously running a car engine at redline – wear and tear are inevitable and accelerated.
- Cardiovascular Disease: Persistent high blood pressure and an elevated heart rate increase the risk of hypertension, atherosclerosis, and other cardiac conditions. The sustained strain on the heart muscle can lead to hypertrophy and reduced efficiency.
- Metabolic Syndrome: Chronic stress can disrupt glucose metabolism, leading to insulin resistance, weight gain (particularly abdominal fat), and an increased risk of type 2 diabetes. The constant mobilization of glucose and suppression of digestion create an imbalance.
- Immune System Dysfunction: While acute stress can temporarily boost the immune response, chronic stress suppresses it. This makes individuals more susceptible to infections, slower wound healing, and potentially increases the risk of autoimmune disorders and certain cancers.
- Gastrointestinal Issues: The chronic suppression of digestive processes can lead to a range of problems, including irritable bowel syndrome (IBS), gastritis, ulcers, and acid reflux. The gut-brain axis, a bidirectional communication pathway, is significantly impacted.
- Musculoskeletal Pain: Persistent muscle tension, particularly in the neck, shoulders, and lower back, is a common symptom. This can contribute to chronic pain conditions, headaches, and migraines.
- Sleep Disturbances: Difficulty falling asleep, frequent waking, and non-restorative sleep are hallmarks of chronic sympathetic activation. The body’s “alarm system” prevents it from entering deep, restorative sleep stages.
Psychological and Emotional Effects
The constant state of hypervigilance and physiological arousal also significantly impacts mental well-being.
- Anxiety Disorders: Chronic SNS activation is a central feature of generalized anxiety disorder, panic disorder, and social anxiety. The body is always primed for danger, leading to excessive worry and apprehension.
- Depression: While seemingly contradictory, chronic stress can deplete neurotransmitters like serotonin and dopamine, contributing to symptoms of depression, including anhedonia (inability to experience pleasure).
- Irritability and Mood Swings: The constant state of tension can lead to increased irritability, impatience, and emotional volatility. Minor frustrations can trigger disproportionate reactions.
- Cognitive Impairment: Chronic stress can impair executive functions such as concentration, memory, decision-making, and problem-solving. This is because the brain’s resources are primarily allocated to threat detection, leaving less capacity for complex cognitive tasks.
- Burnout: Prolonged exposure to stressors without adequate recovery can lead to emotional, physical, and mental exhaustion, a state known as burnout.
Strategies for Releasing the Sympathetic Lock

Reversing a sympathetic nervous system lock requires a multi-faceted approach, focusing on downregulating the SNS and enhancing the activity of the parasympathetic nervous system. It is a process of consciously disengaging the body’s alarm system.
Mindfulness and Relaxation Techniques
These practices directly target the nervous system, promoting a shift from stress to calm.
- Deep Diaphragmatic Breathing: Slow, deep breaths that engage the diaphragm stimulate the vagus nerve, a key component of the PNS. This acts as a direct “off switch” for the SNS. Encourage individuals to practice inhaling slowly through the nose, allowing the abdomen to expand, and exhaling slowly through the mouth.
- Meditation: Regular meditation practice trains the mind to observe thoughts and feelings without getting entangled in them, thereby reducing reactivity to stressors. Various forms, such as mindfulness meditation or transcendental meditation, can be beneficial.
- Progressive Muscle Relaxation (PMR): This technique involves systematically tensing and then relaxing different muscle groups throughout the body. By consciously releasing tension, individuals can teach their bodies to differentiate between states of tension and relaxation.
- Yoga and Tai Chi: These mind-body practices combine physical postures, controlled breathing, and meditation, effectively promoting relaxation and reducing sympathetic tone.
Lifestyle Adjustments
Beyond specific techniques, broader lifestyle changes play a critical role in fostering nervous system balance.
- Regular Physical Activity: While intense exercise can temporarily activate the SNS, regular moderate physical activity helps to regulate stress hormones and improve the body’s ability to recover from stress. It acts as a healthy outlet for built-up tension.
- Adequate Sleep: Prioritizing consistent, restorative sleep is paramount. During sleep, the PNS dominates, allowing for cellular repair and mental processing. Establishing a regular sleep schedule and creating a conducive sleep environment are crucial.
- Nutritional Support: A balanced diet rich in whole foods, fruits, vegetables, and lean proteins helps to stabilize blood sugar levels and provide essential nutrients for nervous system function. Limiting caffeine, alcohol, and processed foods can also be beneficial.
- Nature Exposure (Ecotherapy): Spending time in nature has been shown to reduce stress hormones, lower blood pressure, and improve mood. This is often referred to as “forest bathing” in some cultures.
- Social Connection: Strong social support networks can act as a buffer against stress. Meaningful relationships provide emotional support, validation, and a sense of belonging, all of which contribute to nervous system regulation.
Recent research has shed light on the phenomenon known as sympathetic nervous system lock, a condition that can significantly impact an individual’s stress response and overall health. For a deeper understanding of this topic, you can explore a related article that discusses the implications of sympathetic nervous system dysfunction and its effects on various bodily systems. This insightful piece can be found at XFile Findings, where you will discover more about the intricate connections between stress and physiological responses.
The Role of Professional Intervention
| Metric | Description | Typical Values/Range | Relevance to Sympathetic Nervous System Lock |
|---|---|---|---|
| Heart Rate (HR) | Number of heartbeats per minute | 60-100 bpm (normal resting) | May increase initially during sympathetic activation; can become irregular or suppressed during lock |
| Blood Pressure (BP) | Force of blood against artery walls | 120/80 mmHg (normal) | Elevated during sympathetic activation; may drop or stabilize abnormally during lock |
| Sympathetic Nerve Activity (SNA) | Electrical activity of sympathetic nerves | Varies; measured in bursts per minute | High during activation; may plateau or lock during sustained stress |
| Plasma Norepinephrine Levels | Concentration of norepinephrine in blood | 150-350 pg/mL (resting) | Elevated during sympathetic activation; may remain high during lock |
| Skin Conductance | Measure of sweat gland activity | Variable; increases with arousal | Increased during sympathetic activation; may plateau during lock |
| Respiratory Rate | Breaths per minute | 12-20 breaths/min (normal) | Increases with sympathetic activation; may become irregular during lock |
For individuals experiencing severe or persistent sympathetic nervous system lock, professional guidance may be necessary.
Therapy and Counseling
Various therapeutic modalities can help individuals understand and address the underlying causes of chronic stress and develop coping mechanisms.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and challenge unhelpful thought patterns and behaviors that contribute to stress and anxiety. It equips them with practical strategies for managing stressors.
- Eye Movement Desensitization and Reprocessing (EMDR): This therapy is particularly effective for individuals who have experienced trauma, helping to reprocess distressing memories and reduce their emotional impact on the nervous system.
- Biofeedback: This technique utilizes sensors to provide real-time information about physiological responses (e.g., heart rate, skin temperature, muscle tension). This allows individuals to learn to consciously control these responses and reduce SNS activation.
Pharmacological Approaches
In some cases, medication may be considered as an adjunct to lifestyle changes and therapy, particularly when symptoms are severe and debilitating.
- Beta-Blockers: These medications block the effects of adrenaline, reducing heart rate and blood pressure, thereby dampening the physical manifestations of SNS activation.
- Anxiolytics (Anti-Anxiety Medications): Medications like benzodiazepines can provide short-term relief from acute anxiety symptoms, but long-term use can lead to dependence.
- Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) and other antidepressants can help regulate neurotransmitter imbalances that contribute to anxiety and depression, thereby indirectly influencing SNS activity.
It is crucial to remember that pharmacological approaches should always be prescribed and monitored by a qualified healthcare professional, and they are typically most effective when combined with other therapeutic interventions.
Conclusion
The sympathetic nervous system, while vital for survival, can become a source of chronic distress when locked in a state of perpetual activation. Understanding the mechanisms of the fight or flight response, identifying modern stressors, and recognizing the broad spectrum of physical and psychological consequences are crucial steps. By actively implementing strategies such as mindfulness, lifestyle adjustments, and seeking professional help when needed, individuals can work towards releasing the sympathetic lock and restoring balance to their autonomic nervous system. This journey involves a conscious effort to move from a state of constant alarm to one of greater calm, resilience, and overall well-being. Ultimately, fostering this balance is not merely about individual health but about cultivating a more harmonious relationship between the human organism and its environment.
WATCH THIS 🔥LOST 8 HOURS: What Hospitals Won’t Tell You About Missing Time
FAQs
What is the sympathetic nervous system lock?
The sympathetic nervous system lock refers to a state where the sympathetic nervous system remains persistently activated, leading to prolonged stress responses such as increased heart rate, elevated blood pressure, and heightened alertness. This can occur due to chronic stress or trauma.
What causes the sympathetic nervous system to become locked?
Chronic stress, trauma, anxiety disorders, and certain medical conditions can cause the sympathetic nervous system to become overactive or “locked,” preventing the body from returning to a relaxed state.
What are the symptoms of a sympathetic nervous system lock?
Symptoms may include rapid heartbeat, high blood pressure, excessive sweating, anxiety, difficulty relaxing, muscle tension, and a constant feeling of being “on edge.”
How is a sympathetic nervous system lock diagnosed?
Diagnosis typically involves a medical evaluation including patient history, physical examination, and sometimes tests to assess autonomic nervous system function. Healthcare providers look for signs of prolonged sympathetic activation.
What treatments are available for sympathetic nervous system lock?
Treatment options include stress management techniques, psychotherapy, medications to manage symptoms, relaxation exercises, biofeedback, and lifestyle changes aimed at reducing chronic stress and promoting parasympathetic nervous system activity.
